Abstract
Introduction: AHCT is standard therapy for chemosensitive relapsed DLBCL and survival from the time of AHCT has been well described in large patient cohorts. Outcomes have not been well described for patients who survive a certain time period after transplantation, when the risks of relapse have diminished. We performed a retrospective cohort study to delineate conditional survival in patients with DLBCL who survived 1, 2, and 5 yrs after AHCT. We also compare survival for these cohorts to their general population controls.
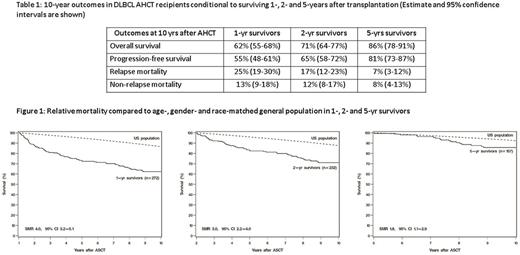
Methods: We included 371 consecutive adult (≥18 yrs) patients with DLBCL who received AHCT at our institution from 2000-2014. 10-year overall survival (OS), progression-free survival (PFS), relapse mortality (RM) and non-relapse mortality (NRM) from AHCT were determined for three cohorts: 1-yr survivors (N=272), 2-yr survivors (N=232), and 5-yr survivors (N=157). Outcomes were estimated with Kaplan-Meier (OS, PFS) or cumulative incidence (RM, NRM). Cox regression analyses were performed to evaluate prognostic factors for OS and PFS. In addition, standardized mortality ratio (SMR) compared to the age-, gender- and race-matched healthy population was estimated for each survivor cohort.
Results: Median age for 1-yr cohort was 56 yrs (19-78 yrs). 61% were male, 78% were stage III/IV and 45% had B-symptoms at diagnosis, 28% had received prior radiation and 81% had received prior rituximab. 77% patients received chemotherapy mobilization and Bu/Cy/VP was conditioning regimen for 97% patients. Median followup for this 1 yr cohort was 8 yrs (1.3-16.5 yrs). OS, PFS, RM and NRM at 10 yrs after AHCT are described in Table 1. OS and PFS improved with increasing survival after transplantation. Relapse was the primary cause of death in 1- and 2-yr survivors; cumulative incidence of RM and NRM was low but similar in 5-yr survivors. As expected, in multivariable analyses, lymphoma relapse prior to landmark time was associated with significantly worse OS and PFS for 1-, 2- and 5-yr survivors. Among other patient and disease characteristics evaluated in risk factor analysis, age and duration of AHCT hospitalization were the only factors associated with OS and PFS. Older age (10 yr increments) was associated with greater mortality risk among 1- and 2-yr but not 5-yr survivors. Older age at AHCT was associated with worse PFS in all three survivor cohorts. Prolonged hospital stay, as a surrogate for early post-transplant complications, was also associated with lower OS for all three cohorts, and lower PFS for 2-yr and 5-yr survivors. Survival was lower compared to the general population, although it improved and approached that of healthy peers with increasing post-transplant survival (SMR 4.0, 3.0 and 1.8 among 1-, 2- and 5-yr survivors, respectively, Figure 1).
Conclusions: Conditional OS and PFS for DLBCL patients treated with AHCT improves with increasing survival post-transplantation. Relapse is the primary driver of poor survival, although the probability of death due to relapse decreases over time. NRM continues to be an important cause of treatment failure even among patients surviving 5-years after AHCT. Our data provide personalized survivorship information for DLBCL AHCT recipients and identify risk factors for poor survival. Our study also underscores the need for continued research on decreasing relapse risk and for surveillance for prevention and management of late-complications in this population.
Kharfan-Dabaja: Incyte: Speakers Bureau; Alexion Pharmaceuticals: Speakers Bureau; Seattle Genetics: Speakers Bureau. Majhail: Anthem, Inc.: Consultancy; Sanofi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal